MICROBIOLOGY CULTURE INSTRUCTIONS Microbiology Programs
Inspect the fiberboard container carefully for all inclusions. After inventorying the contents of the container, store them in a refrigerator. These instructions are illustrated in the Program Guide online under Microbiology Instructions.
Special Safety Precautions - These specimens contain pathogens or potential pathogens and should be considered infectious and handled as though they are capable of transmitting disease. They should be handled and disposed of only by personnel trained to work with pathogenic bacteria. All laboratory precautions and safety measures appropriate to handling live cultures should be practiced when working with these specimens.
In addition to the Precautions section of the program guide, be especially careful to avoid aerosol creation, inhalation, ingestion or injection of bacteria. These specimens should be disposed of as hazardous waste.
Rehydration Instructions for Swab Samples – These specimens are stabilized viable microorganisms lyophilized directly to an inoculation swab. A Rehydration Fluid tube is provided for each swab. The Microbiology Rehydration Fluid is located with the rest of your samples and is not found inside the tube with the swabs. The Diluent vials are placed in a pouch labeled REHYDRATION FLUID. There are up to 5 equivalent vials, each containing approximately 0.5 mL of TSB. The vials are not specifically labeled for any sample or Microbiology program module. We recommend you label the rehydrating vial prior to use to avoid confusion.
a. Warm appropriate amount of media, one specimen swab and one vial of rehydrating fluid to room temperature (20-25ºC) for each specimen tested. Store the second swab and extra rehydrating fluid vials in the refrigerator in case repeat testing is necessary.
b. Remove swab from plastic tube and submerge the sample portion into the fluid. Allow approximately 10 seconds for the lyophilized specimen to liquify while mixing and swirling the swab gently.
c. Once the swab is saturated, inoculate your media directly with the swab. Return the swab to the rehydration fluid before inoculating each subsequent culture plate.
d. If you perform a gram stain as part of your identification procedure, you can now transfer a portion of the liquified specimen to a clean glass slide. Be sure to have inoculated all culture media prior to using the specimen swab to prepare your gram stain. NOTE: There will be a small amount of charcoal residue from the lyophilization process present on your gram stain slide. This should not interfere with your ability to determine the staining pattern of the organism.
e. Continue by following the procedure and methods used by your lab to identify the organism(s) present in these specimens.
For Uricult users or users of other tests that require a liquid sample.
a. Open each foil pouch at the tear slit and remove the swab from the foil pouch.
b. Submerge the swab portion only into the provided rehydration broth tube for 30 seconds to wet the swab.
c. Express as much material from the swab as possible by firmly pressing the head of the swab against the side of the rehydration broth tube.
d. Swirl the rehydration broth tube gently to ensure even mixing and then use the broth as you would a liquid sample.
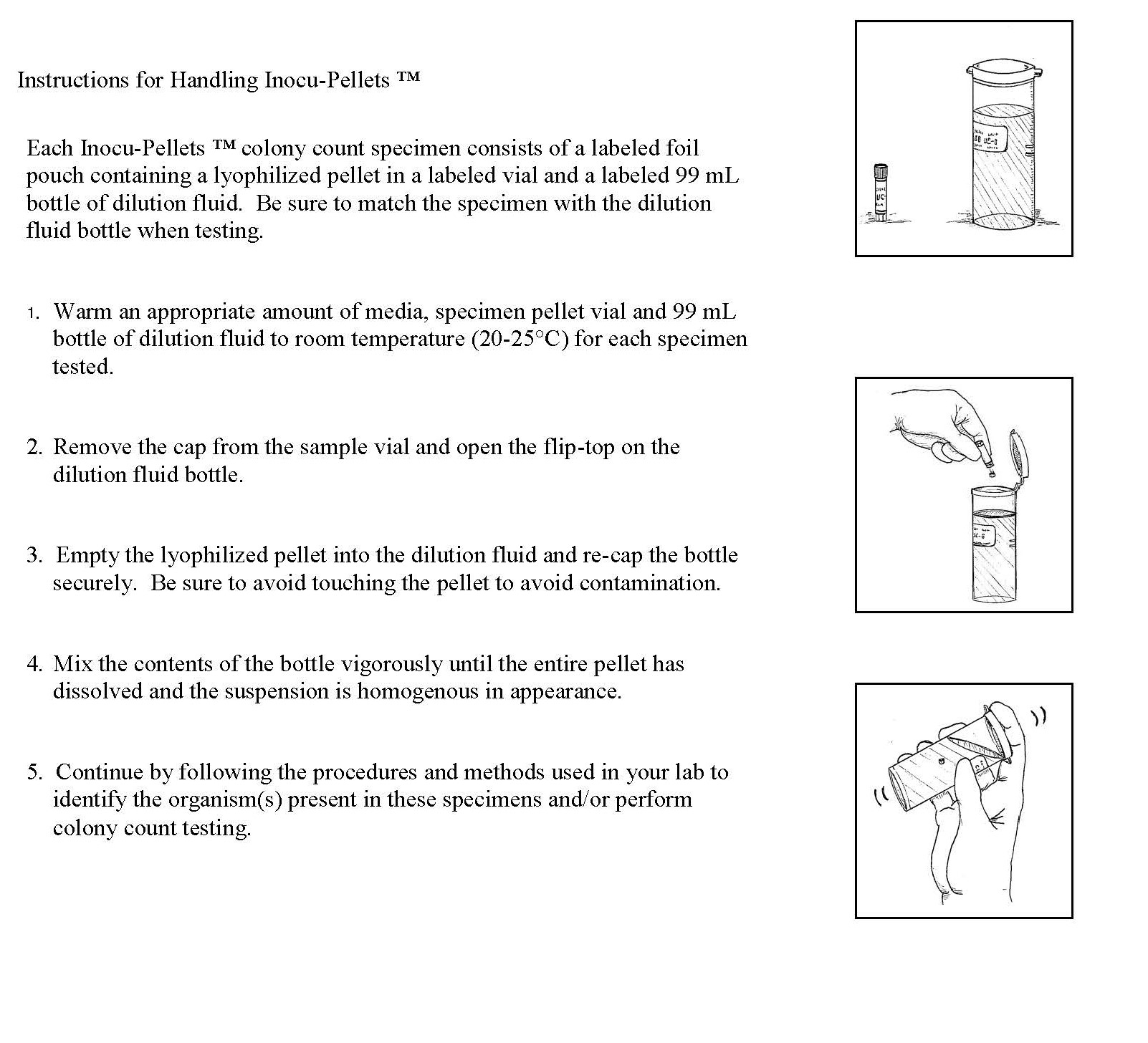
Urine Colony Count (CC-) Samples – Each sample consists of lyophilized pellet in a labeled foil pouch and a labeled 99 mL bottle of dilution fluid.
a. Warm an appropriate amount of media, specimen pellet and 99 mL bottle of dilution fluid to room temperature (20-25ºC) for each specimen tested.
b. Remove the cap from the sample vial and open the flip-top on the dilution fluid bottle.
c. Empty the lyophilized pellet into the dilution fluid and recap the bottle securely. Be careful to avoid touching the pellet to avoid contamination.
d. Mix the contents of the bottle vigorously until the entire pellet has dissolved and the suspension is homogeneous in appearance.
e.The entire contents of the dilution bottle (which now contains the dissolved lyophilized pellet) simulates a urine sample.
Proceed to test as you would a patient sample in your laboratory.
f. Continue by following the procedures and methods used by your lab to identify the organism(s) present in these specimens and/or perform colony count testing.
g. If you perform a gram stain as part of your identification procedure, you may transfer a small amount of the mixed solution from the first CC specimen to a clean glass slide. Be sure to use sterile technique when transferring the solution. NOTE: There will be a small amount of charcoal residue from the lyophilization process present on your glass slide. This should not interfere with your ability to determine the staining pattern of the organism.
h. Record your colony count results for only the first two CC specimens.
Determining Type (Extent) of Laboratory Service - All participants, regardless of the extent of their laboratory practice, evaluate the same specimens. In order to be graded appropriately, you must report the extent of laboratory practice (Extent 0, 1, 2, 3, 4 or 5) for each specimen. Refer to the Program Guide online to determine your extent.
1. Subject each specimen to your protocol for each source as described at each specimen number on your reporting form.
2. Based on what you would report in the context of your specific laboratory practice, determine your extent for each specimen independently of each other, according to the definitions on the reporting form and clarified in the following table:
Results Reported |
Extent |
of |
Laboratory |
Service |
||||||
0 |
1 |
2 |
3 |
4 |
5 |
|||||
Gram Stain |
must not report |
must report |
may report |
may report |
may report |
may report |
||||
Antigen Screen |
must not report |
may report |
must report |
may report |
may report |
may report |
||||
Susceptibility Testing (ASTs)* |
may report |
may report |
may report |
may report |
may report |
may report |
||||
Identification of Genus Only |
must not report |
may report |
may report |
must report |
must not report |
must not report |
||||
Speciation of Aerobes |
must not report |
may report |
may report |
may report |
must report |
must report |
||||
Detection of Anaerobes |
must not report |
may report |
may report |
may report |
must report |
must report |
||||
Identification of Anaerobes |
must not report |
may report |
may report |
may report |
may report |
must report |
||||
*Reporting ASTs applies only to Specimen 1 and assumes the use of pure isolates. Participants performing ASTs without identifications, even presumptive ones, must use Extent 0 to avoid being given a score of zero for missing culture results |
||||||||||
Regardless of the extent reported, we are required to grade the most definitive identification reported. This means, for example, that a species result takes precedence in grading over a genus, antigen or Gram stain result.
If unable to decide between extents for a given specimen, report the lowest extent, which applies, except Extent 0. In order to preserve the opportunity to get a zero on one specimen and still receive 80 percent overall, it is advisable to avoid using Extent 0 when Gram stain (Extent 1) or antigen screening (Extent 2) results are available for reporting. It is acceptable to challenge your Gram stain or antigen screening procedure(s) with our bacteriology specimens (without regard to specimen source information) in order to receive five specimen scores upon which to generate an overall procedure score for bacterial identifications. We are required to categorize participants who fail to report their extent(s) as Extent 5 and to grade accordingly.
Coding for Presumptive Culture Identification (or other screening methods) - Participants reporting presumptive identifications by culture must not use result codes 726 to 911. If performing isolations only with selective media, these participants might need to report code 948 (No pathogen isolated), but should not report either code 949 (No aerobic growth) or 951 (No aerobic or anaerobic growth).
When using a presumptive culture or other screening methods for identification, be certain to respond using result codes appropriate for the origin of the sample being tested; result codes >911. CMS is particularly concerned that laboratories performing limited testing report their results in such a way as to reflect knowledge of the limitations of their method. Therefore, do not use codes such as 948 (no pathogens found) if your laboratory does not screen for GC on throat cultures, Campylobacter on stool cultures and so on. You MUST select a code that accurately reflects the limitations of your testing or you will be scored as incorrect.
Coding Extent 3, 4 and 5 Results - For the first four Specimens in each event, participants using Extent 3, 4 or 5 may report only the organism(s), which they consider to be the significant pathogen(s) that is/are clearly responsible for the illness described, excluding immuno-compromised patients. CLIA directs that we require reporting of all organisms present for at least one sample which contains multiple organisms. The last Specimen in each event will contain multiple organisms and may contain multiple pathogens. If you report extents 3, 4 or 5, you must report all organisms present or you will be flagged for an incorrect response. The significant pathogen must be reported as organism #1 when multiple organisms are detected.
Code your answers using the Organism Result Code list on the reveres side of these instructions. Anti-microbial susceptibility tests (ASTs) are to be performed on the most significant pathogen in first specimen only, using the AST codes listed on the reverse side of these instructions. Per CMS requirements participants will be flagged for inappropriate selection of Antimicrobial Agents as listed in the current edition CLSI (NCCLS) guidelines and M100. Selection of an incorrect Antimicrobial will be scored incorrect.
Refer to your reporting form for specimen sources and other reporting requirements. If you do not see a particular Anti-microbial Agent listed, please attach a note indicating that you would like for us to add a code for that agent. Note: We will not add any new Anti-microbials until they are listed in the CLSI guidelines.
Please review codes. Changes have been made to the organism codes.
738 |
Acinetobacter sp. |
807 |
Haemophilus influenzae |
872 |
Staphylococcus lugdunensis |
THROAT CULTURE RESULT CODES |
|
740 |
Acinetobacter baumannii |
809 |
Haemophilus parahaemolyticus |
900 |
Staphylococcus pseudintermedius |
919 |
Neg for beta-hemolytic Grp A strep screen |
739 |
Acinetobacter lwoffii |
810 |
Haemophilus parainfluenzae |
879 |
Staphylococcus saprophyticus |
921 |
Pos for beta-hemolytic Grp A strep screen |
766 |
Achromobacter sp. |
811 |
Klebsiella sp. |
890 |
Staphylococcus simulans |
922 |
Neg for Grp A strep by culture |
758 |
Achromobacter xylosoxidans |
812 |
Klebsiella aerogenes |
867 |
Stenotrophomonas sp. |
923 |
Pos for Grp A strep by culture |
741 |
Aerococcus sp. |
813 |
Klebsiella oxytoca |
932 |
Stenotrophomonas maltophilia |
920 |
Presumptive Pos for Grp A strep by culture |
743 |
Aerococcus urinae |
814 |
Klebsiella pneumoniae |
881 |
Streptococcus sp. |
927 |
Neg for Grp A strep; not screened for GC |
742 |
Aerococcus viridans |
815 |
Lactobacillus sp. |
883 |
Streptococcus sp.; alpha-hemolytic |
943 |
Aerobe found, but referred for ID |
746 |
Aeromonas sp. |
820 |
Lactobacillus casei |
889 |
Streptococcus sp.;beta-hemolytic; not Grp A |
947 |
No aerobic growth on blood agar |
747 |
Aeromonas hydrophila |
817 |
Listeria sp. |
892 |
Streptococcus sp. Group C - large colony |
948 |
No pathogens isolated |
749 |
Alcaligenes sp. |
818 |
Listeria monocytogenes |
893 |
Streptococcus sp. Group C - small colony |
949 |
No aerobic growth |
748 |
Alcaligenes faecalis |
819 |
Micrococcus sp. |
894 |
Streptococcus sp.; Group D |
||
752 |
Anaerococcus sp. |
821 |
Micrococcus luteus |
882 |
Streptococcus sp.; non-hemolytic |
URINE CULTURE RESULT CODES |
|
755 |
Anaerococcus prevotii |
751 |
Moellerella sp. |
898 |
Streptococcus agalactiae |
993 |
Presumptive gram-negative organism |
750 |
Bacillus sp. |
754 |
Moellerella wisconsensis |
794 |
Streptococcus anginosus |
994 |
Presumptive gram-positive organism |
753 |
Bacillus cereus |
822 |
Moraxella sp. |
899 |
Streptococcus bovis group |
943 |
Aerobe found, but referred for ID |
756 |
Bacillus subtilis |
823 |
Moraxella catarrhalis |
885 |
Streptococcus constellatus |
948 |
No pathogens isolated |
760 |
Bacteroides sp.; B. fragilis group |
774 |
Moraxella lacunata |
903 |
Streptococcus dysgalactiae |
949 |
No aerobic growth |
759 |
Bacteroides sp.; not B. fragilis group |
833 |
Moraxella osloensis |
891 |
Streptococcus gallolyticus |
||
761 |
Bacteroides fragilis |
824 |
Morganella morganii |
895 |
Streptococcus intermedius |
GENERAL RESULT CODES |
|
744 |
Burkholderia sp. |
825 |
Neisseria sp. |
876 |
Streptococcus mitis |
943 |
Aerobe found, but referred for ID |
745 |
Burkholderia cepacia |
856 |
Neisseria cinerea |
896 |
Streptococcus mutans |
944 |
Anaerobe found, but referred for ID |
763 |
Campylobacter sp. |
826 |
Neisseria gonorrhoeae |
901 |
Streptococcus pneumoniae |
946 |
Anaerobic cultures not performed - refer |
762 |
Campylobacter coli |
829 |
Neisseria meningitidis |
887 |
Streptococcus pyogenes |
||
764 |
Campylobacter fetus |
832 |
Neisseria mucosa |
904 |
Streptococcus salivarius |
720 |
Gram negative bacilli |
765 |
Campylobacter jejuni |
827 |
Neisseria sicca |
902 |
Streptococcus sanguinis |
721 |
Gram negative coccobacilli |
767 |
Citrobacter sp. |
788 |
Neisseria subflava |
897 |
Streptococcus viridans group |
722 |
Gram negative diplococci |
768 |
Citrobacter braakii |
836 |
Pantoea sp. |
905 |
Vibrio sp. |
723 |
Gram positive bacilli |
769 |
Citrobacter freundii |
839 |
Pantoea agglomerans |
907 |
Vibrio parahaemolyticus |
724 |
Gram positive cocci |
770 |
Citrobacter koseri |
727 |
Parabacteroides sp. |
906 |
Vibrio vulnificus |
725 |
Gram positive diplococci |
772 |
Clostridioides difficile |
726 |
Parabacteroides distasonis |
909 |
Yersinia sp. |
||
771 |
Clostridium sp. |
733 |
Pasteurella sp. |
910 |
Yersinia enterocolitica |
945 |
No anaerobes isolated |
773 |
Clostridium perfringens |
732 |
Pasteurella multocida |
911 |
Yersinia pseudotuberculosis |
947 |
No aerobic growth on blood agar |
775 |
Clostridium septicum |
729 |
Pediococcus sp. |
GENITAL CULTURE RESULT CODES |
948 |
No pathogens isolated |
|
777 |
Corynebacterium sp. |
728 |
Pediococcus acidilactici |
722 |
Gram negative diplococci |
949 |
No aerobic growth |
779 |
Corynebacterium jeikeium |
830 |
Peptostreptococcus sp. |
995 |
Gram negative diplococci absent |
951 |
No aerobic or anaerobic growth |
782 |
Corynebacterium striatum |
831 |
Peptostreptococcus anaerobius |
913 |
Neg for N. gonorrhoeae by culture |
950 |
Non-pathogenic aerobe found, no anerobic |
784 |
Corynebacterium ulcerans |
840 |
Plesiomonas sp. |
914 |
Pos for N. gonorrhoeae by culture |
work up performed |
|
783 |
Corynebacterium urealyticum |
924 |
Plesiomonas shigelloides |
915 |
Presumptive for N. gonorrhoeae, would refer |
||
785 |
Corynebacterium xerosis |
731 |
Prevotella sp. |
961 |
Neg for N. gonorrhoeae antigen |
718 |
Normal flora present |
781 |
Cronobacter sp. |
730 |
Prevotella bivia |
962 |
Pos for N. gonorrhoeae antigen |
988 |
Contaminated Specimen |
780 |
Cronobacter sakazakii |
834 |
Proteus sp. |
917 |
No growth on Thayer Martin |
960 |
Other organism not listed |
776 |
Cutibacterium sp. |
835 |
Proteus mirabilis |
918 |
Growth on Thayer Martin, would refer |
||
786 |
Cutibacterium acnes |
837 |
Proteus vulgaris |
943 |
Aerobe found, but referred for ID |
||
796 |
Eikenella sp. |
847 |
Providencia sp. |
949 |
No aerobic growth |
||
790 |
Eikenella corrodens |
843 |
Providencia rettgeri |
STOOL CULTURE CODES |
|||
793 |
Elizabethkingia sp. |
848 |
Providencia stuartii |
718 |
Normal flora present |
||
816 |
Elizabethkingia meningoseptica |
838 |
Pseudomonas sp. |
930 |
Normal flora present; no enteric pathogens isolated |
||
787 |
Enterobacter sp. |
841 |
Pseudomonas aeruginosa |
931 |
Neg for Sal, Shig, Vib, Yers & Campy |
||
789 |
Enterobacter cloacae |
842 |
Pseudomonas fluorescens |
933 |
Neg for Sal, Shig, Yers & Campy |
||
791 |
Enterococcus sp. |
844 |
Pseudomonas luteola |
(referred for Vibrio culture) |
|||
792 |
Enterococcus faecalis |
845 |
Pseudomonas stutzeri |
934 |
Neg for Sal, Shig,Yers & Vib (ref for Campy) |
||
795 |
Enterococcus faecium |
846 |
Salmonella sp. |
935 |
Neg for Sal, Shig & Vib |
||
797 |
Enterococcus gallinarum |
858 |
Salmonella sp.; Group D |
(referred for Yers & Campy culture) |
|||
737 |
Erysipelothrix sp. |
850 |
Salmonella enterica spp. |
937 |
Neg for Sal, Shig & Campy |
||
736 |
Erysipelothrix rhusiopathiae |
852 |
Salmonella enteritidis |
(referred for Vib & Yers culture) |
|||
798 |
Escherichia sp. |
851 |
Salmonella typhi |
939 |
Neg for Sal, Shig & Yers |
||
799 |
Escherichia coli |
862 |
Serratia sp. |
(referred for Vib, Campy culture) |
|||
888 |
Fannyhessea sp. |
863 |
Serratia liquefaciens |
940 |
Neg for Sal,Shig,Vibrio&Campy (ref for Yers) |
||
778 |
Fannyhessea vaginae |
865 |
Serratia marcescens |
941 |
Neg for Sal & Shig |
||
735 |
Finegoldia sp. |
866 |
Shigella sp. |
(referred for Vib, Yers & Campy culture) |
|||
734 |
Finegoldia magna |
870 |
Shigella boydii (Serotype C) |
943 |
Aerobe found, but referred for ID |
||
800 |
Fusobacterium sp. |
869 |
Shigella flexneri (Serotype B) |
944 |
Anaerobe found, but referred for ID |
||
804 |
Fusobacterium necrophorum |
871 |
Shigella sonnei (Serotype D) |
945 |
No anaerobes isolated |
||
801 |
Fusobacterium nucleatum |
873 |
Staphylococcus sp. |
948 |
No pathogens isolated |
||
802 |
Gardnerella sp. |
874 |
Staphylococcus sp.; coagulase-negative |
949 |
No aerobic growth |
||
803 |
Gardnerella vaginalis |
875 |
Staphylococcus sp.; coagulase-positive |
951 |
No aerobic or anaerobic growth |
||
828 |
Granulicatella sp. |
877 |
Staphylococcus aureus |
||||
808 |
Granulicatella adiacens |
878 |
Staphylococcus epidermidis |
||||
805 |
Haemophilus sp. |
880 |
Staphylococcus haemolyticus |
||||
806 |
Haemophilus haemolyticus |
884 |
Staphylococcus hominis |
Instructions for Handling INOCU-SWAB II™

Instructions for Handling INOCU-PELLETS